In this article we present a strange clinical case of a 53 years old man with severe neuropsychiatric acute syndrome. The patient is a well succeeded 53 years old business man, married, father of two adult male sons. In 12 months, a tragic neuropsychiatric picture was developed, and changed his life dramatically.
Case report. A strange case of a lousy mind in a “perfect” brain. Early pseudodementia, frontotemporal dementia, or nothing at all?
Luis Maia, PhD. Cédula Profissional da Ordem dos Psicólogos, n.º 102. Auxiliar Professor - Beira Interior University. Clinical Neuropsychologist, PhD (USAL - Spain). Neuroscientist, MsC (Medicine School of Lisbon - Portugal). Medico Legal Perit (Medicine Institute Abel Salazar - Oporto, Portugal). Graduation in Clinical Neuropsychology (USAL - Spain). Graduation in Investigative Proficiency on Psychobiology (USAL - Spain) Clinical Psychologist (Minho University - Portugal)
In this article we present a strange clinical case of a 53 years old man with severe neuropsychiatric acute syndrome. The patient is a well succeeded 53 years old business man, married, father of two adult male sons. In 12 months, a tragic neuropsychiatric picture was developed, and changed his life dramatically.
Seven years ago, but with increased incidence in the last year, the patient presented progressive deficits in operating executive functions and memory. Such deficits extended beyond events whose mnesic information could be considered as long-term, like omissions of concrete situations and experiences in the last days, weeks and even months (autobiographical memory).
This aspect provoked a worsening in his professional responsibilities (the patient is the main founder of a large company of house isolation and overheating). This is reflected in unthinkable mistakes for his normal performance, such as making incorrect measurements, forget to comply with labor commitments (e.g. forget large orders of great financial profit), shouting out loud with employees, misplacing his own responsibilities about errors committed (e.g. usually responsibility for certain loss that have occurred are attributable to itself, but in his opinion, his employees are the ones to be blamed, etc).
Overall, the patient becomes currently described by his family as childish (uses slang and inappropriate speech in front of customers and employees – this pattern does not seems to be his normal way to behave), exaggerated when defeated (e.g. forced an employee to use a cutter in a scrap of a vehicle which still had petrol and, despite the employee had called unceasingly, he forced him to use the tool, which led to vehicle went in flames, jeopardizing their integrity).
In such situation, he does not presented signs of fear and do not attempted to protect himself. Instead, took a further exasperated attitude with the employee, blaming him by the accident despite the proximity of flame and imminent risk of explosion. Similarly, responds inappropriately to what he is asked, and states that is only due to an obvious marked deficit at the level of bilateral hearing acuity (diagnosed by a specialist physician).
As a family management company (e.g. wife take care of accounting, the eldest son treats of contacts with customers, etc.) the patient presents an aggressive and humiliation behavior of family members, especially the eldest son (described by his mother as a responsible and worker person), without demonstrating discomfort with the presence of employees or customers (this completely abnormal behavior is recent in his past).
He also presents an irresponsible and inconsistent attitude. For example, having to drive heavy vehicles with chemical reagents, he often has small roadside accidents (up to now without consequences). He justify (with an infantile attitude): "Satan is my friend … he pulls me out of road (sic.)".
The wife says that, at least in three occasions, the patient entered handling vehicles in forbidden way, in traffic circle, causing great danger to him and to other drivers.
Common in each of the above-described situations is that, according to the family, when called attention to the risks, he presents an inconsistent attitude, do not seeming to present any insight of their actions dangers.
He doesn’t seem to present severe depressive symptoms. What frequently occur, is to pass considerable amounts of times lost in her own thoughts without expressing any significant attitude or behavior (“I am able to be half an hour looking for room clock without saying anything to anybody” sic.).
As a relevant aspect, it seems to us that slight changes occurred in his basic hygiene and care pattern in daily life activities. Although a significant change cannot be considered in terms of carelessness and lack of hygiene, he presents a care decrease in shaving and bathing frequency (passed from a daily based activity to 2 or 3 times per week).
Unlike his past history, he became disorganized about cleaning his own mess. Present stressed hyper-phagia and reduced libido, with absence of sexual intercourse at least for four years.
Displays monetary loosening with unnecessary expenses, without appear to commit such acts during a maniac or hypo-maniac episode. For example, on agriculture properties, that he is the owner, have already invested in four tractors vehicles and other medium-large machinery highly expensive (it should be noted that this activity is not used for commercial profit, but solely by hobby and family consumption). He also tends to borrow large machinery and cannot remember who loaned them and, because it is not returned, blame families and employees for such errors.
As a corollary of what was referred above, his wife states, "this last year was of total decadence” (sic.).
He ultimately recurred to our services were, after extensive neuropsychological evaluation and anamnesis assessment, his case seemed better explained by progressive frontal cortical degeneration. Particularly, the patient has been affected in recent years (seven years) by symptomatology indicative of frontal temporal syndrome, with a clear worsening in the last 12 months.
Neuropsychological assessment
The subject was profoundly evaluated with several neuropsychological batteries, in three different moments during the years 2009 and 2010.
Despite the results found, since the beginning, the patient presented strong alterations in learning and memory. Anterograde amnesia, neuropsychiatric signals, as alterations of personality, slang language, obscene behavior (extra marital relationships), lack of social conscience, strong irresponsibility (for example: driving a car in a forbidden way, with low sense of responsibility, hiperphagia, hypersomnolece, etc).
The first clinical hypotheses about this developing syndrome was Mild Cognitive Impairment, of Frontal–Temporal type, undoubtedly of degenerative evolutive frame.
Particularly, the major deficits in Neuropsychological areas and Neuropsychiatric symptoms that the patient shows are, as follows: a) The patient was first evaluated by a psychiatrist who allegedly, according to his wife and himself, was diagnosed with dementia of Alzheimer's type, on a single inquiry, without any diagnostic auxiliary means; b) Once he got worse she looked for a Neurologist that diagnosed a severe depression and, allegedly said: “you have a problem of soul and I don’t understand you"; c) The family finally came to our services.
Summary of Neuropsychiatric Data
MSSE: 27 points, in 30 possible; nine grade of schoolarity (primary school).
In Complex Rey Figure the subject shows a slightly deficit in re-evocation of visual-constructive material (re-evoking only some particularities of the previously submitted image). However, we can see that the small errors committed are directly related to monitoring deficits and attention focus in the organization, integration, and building an image as a whole.
In bimanual coordination capacity (conflictive go-no-go tasks – alternate hand positions simultaneously) the patient shows significant bad performance characterized by uncoordinated movements with incidence in upper left distal member. When asked to perform tasks by increasing speed, difficulties also seem to be incremented.
Finally, in verbal fluency the patient presents unsatisfactory performances in pronunciation and slowing thought (Bradiphrenia).
Other clinical data
Tumor Markers
Although there is history of prostatic inflammation, tumoral markers do not show any relevant factor to the comprehension of the entire case.
Genetic Study
Negative for Psen1, Psen2, mapt & prgn.
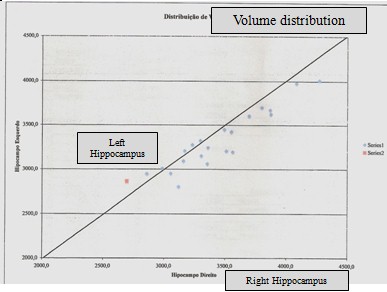
Hippocampus Volumetric Study
After a process of normalization and compared with normal healthy population for the hipocampal formations, the showed values are slight out of the defined normalized area, with a more reduced concentration in right hippocampus (see images below).
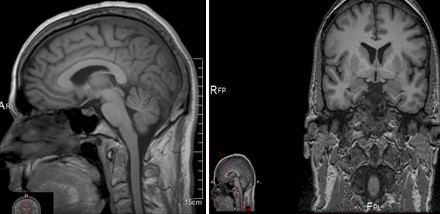
Left Sagital hemisphere & Frontal temporal coronal section
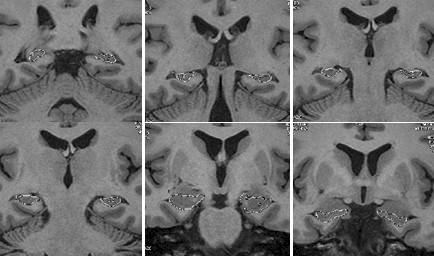
It is also in accordance with the idea that this relative process of atrophy of hypocampal formation affects mainly the respective bodies, with less significance in the hipocampal heads.
It is stated that in the valorization of these results, it has to be considered a slight bad proportion between the atrophic patterns of limbic formations, compared with the level of encephalic cortical atrophy (see images below).
Coronal sections of Hippocampus formation
(Volumetric sections from head & body – corpus callosum)
Graphic of volumetric measurements from bilateral Hippocampus formation
Electroencephalography
The results suggest etectrogenises constituted by Alpha activity with 10Hz frequency, medium amplitude, symmetric with predominance of posterior derivations. Activations by hyperventilation don not provoke pathologic graphic elements. Major Results: trace without signals of pathologic activity.
Magnetic Resonance results
Normal spaces sulci-cinstern and ventricular space in both intracranial compartments, in terms of permeability, configuration and dimensions. Focal asymmetries are not found. Regarding to signal presented, cerebral parenquima do not present considerable alterations. Some spaces of Virchow should be considered with no relevance.
A more detailed study, focused on hipocampal formations and rest of temporal lobes shows a reduced volumetric structure, mostly in the body of hippocampus and particularly at the right hemisphere. It is also observed a minor hiposignal in the Fast Flair Sequence (T2), at hippocampus level.
PET SCAN
In the PET Scan Study we can see a generalized cortical reduction on captation of radiopharmac, partially preserved in visual occipital cortex and in basal ganglia as well as in thalamic nucleus. We do not found regional deficits suggestive of Alzheimer Disease or Frontal Temporal Dementia.
Although the pattern found of cortical hiphometabolism, with preservation of visual cortical cortex are not typical for AD or FTD, degenerative microangiopathic and / or encephalitic pathology could not be excluded.
General clinical conclusions
The patient presented some deviant values in some clinical parameters but nothing that could justify the dramatic clinical picture. The only clinical examination not pursed was a cerebral biopsy due the very intrusive nature of this procedure.
The patient is undoubtedly disorganized in his capacity to cope with daily life responsibilities (not only socially but familiarly speaking). His ability to work was profoundly reduced, and a neuropsychiatric frontal-temporal syndrome is unquestionably present (despite the unknown ethiopatogeny).
This intriguing clinical case must, by that, be strongly discussed.
Discussion
One of the first hypotheses in the comprehension of this case is to consider if we were dealing with an unusual case of early pseudo dementia. Let us look at it.
The term pseudo dementia was first utilized by Wernicke, related with cases that comprised chronically hysterical states, as stressed by Bleuler (1934, in Bulbena & Berrios, 1986).
Nussbaum (1994) states that this term, “ pseudodementia” has remained a permanent nosological entity in the literature for over 100 years. He states that the identification of the fact that clinical symptoms related with reversible neuropsychiatric circumstances could imitate permanent disorders is accepted since the middle of the 19th century. As the author states: “The importance of the term lies in the inherent assumption that the presenting dementia is not real, or is at least reversible, and therefore treatable. Nonetheless, there continues to be controversy regarding the validity and appropriate clinical use of the term” (p.71).
Jones, Tranel, Benton & Paulsen (1992) made neurological evaluations in 37 patients (older than 45 years) showing early and subtle alterations changes in memory, in order to explore the efficacy of several neuropsychological tests in the distinction among dementia and pseudo - dementia. With a six months interval of “test” “re – test” the authors found major relations between faulty temporal orientation, visuo construction, and visual memory at Time 1, and the subsequent development of dementia.
There were noteworthy correlations between clinical result and Time 1 performances on a temporal orientation questionnaire, the Revised Visual Retention Test, and the Block Design subtest of the Wechsler Adult Intelligence Scale—Revised (WAIS—R). They state that a suitable weighting of these measures in neuropsychological judgment may assist in the differential diagnosis of dementia and pseudo dementia. Important to our present case is that the utilization of some tests could not solve the necessity to reach novelty and multidimensional nature of the discriminating tasks that may account for this effect.
This case, as one of my Neurologist colleague called, was a hard one to understand.
We find it interesting to share these data because, from time to time, some patients came to us, we provide all knowledge and technological help in order to identify what is happening with the patient, but, even though, it seems not being enough.
This case stresses the necessity of interdisciplinary work in clinical evaluation and treatment.
The patient continues to come to sessions of Neuropsychological and Psychotherapeutic help (in a family centered way), and soon, we will deliver data from the reassessment of this strange case of neuropsychiatry marked reality.
References
Bulbena, A. & Berrios, G.E. (1986). Pseudodementia: facts and figures. The British Journal of Psychiatry. 148, 87-94.
Jones, R.D., Tranel, D., Benton, A. & Paulsen, J. (1992). Differentiating dementia from "pseudodementia" early in the clinical course: Utility of neuropsychological tests. Neuropsychology. 6(1, Jan), 13-21.
Nussbaum, P.D. (1994). Pseudodementia: A slow death. Neuropsychology Review. 4 (2, June), 71-90.