Spontaneous rupture of a giant hepatic hemangioma, case report and literature review .1
Spontaneous rupture of a giant hepatic hemangioma, case report and literature review
Víctor Gómez Recillas *
Jesús Ocádiz Carrasco *
Jose Onofre Lopez Vite*
José Manuel Nogueira Fernandez **
Jaime Santos Hernandez **
José Luis Hernández Ortega ****
* General surgery resident Nuevo Sanatorio Durango
** General Surgeon Nuevo Sanatorio Durango
*** Radiology Department Chief
**** President of the International College of Surgeons, Northamerican Federation, Mexico chapter
Medical center Nuevo Sanatorio Durango
Spontaneous rupture of a giant hepatic hemangioma
Summary
Hepatic hemangioma is the most common benign tumor of the liver. The vast majority are asymptomatic and diagnosed as occasional findings in imaging studies. Only 1% may complicate with spontaneous rupture with a high mortality rate. Until date, very few cases have been reported with a good operative outcome. We present the case of spontaneous rupture of a giant hepatic hemangioma in a 17 year old male presenting with abdominal pain and shock due to hemoperitoneum. Patient was successfully managed by urgent abdominal exploration with packing of liver bleeding. Selective arterial embolization of right hepatic artery was successfully made in mediate postoperatory with good clinical outcome. Definitive surgical hepatic resection should be made with a better prognosis due to the previous arterial embolization.
Key words: Giant Hepatic Hemangioma, Hemoperitoneum, Selective arterial embolization
Introduction
Natural history of hepatic hemangiomas shows that near 80% will keep their original size whereas 1% presents growth. Spontaneous rupture is something exceptional and it is more often associated with sizes bigger than 5 cm. (1,2,3) Literature review shows a high mortality rate in the reported cases of spontaneous rupture with surgical management. Until date only five adult patients from 32 published cases have survived. (3,13) The case we are presenting may be the sixth reported case of survival after surgical and embolization management. Once the hemangioma is broken the unexpected hepatic resection of the lesion is recomended to those stable patients with less risk of morbidity, while unstable patients must be treated with arterial hepatic embolization prior to resection. (11,13) We present the case of a 17 year old patient with abdominal pain and shock due to spontaneous rupture of a giant hepatic hemangioma. The patient was successfully managed with perihepatic packing followed by hepatic arterial selective embolization.
Case report
A 17-year-old man was admitted in a primary care center, suffering nausea, vomiting and fainting, he was treated with intravenous fluids and oral vasoconstrictor because of hypotension, he was discharged without a clear diagnosis and began with acute abdominal pain in the right dorsal region, vomiting, anuria and struggle. He was readmitted with empiric antibiotic treatment for urinary tract infection due to proteinuria and hematuria. Abdominal ultrasonography reported several nodules in hepatic parenchima suggesting abscess; for which treatment with ceftriaxone and metronidazole was initiated. Patient showed symptom improvement and a new ultrasonography was made five days after reporting partial resolution of liver lesions. On the sixth day the patient began with acute abdominal pain located to right upper quadrant, fainting, abdominal distention and shock without previous traumatic antecedent. He underwent urgent laparotomy suspecting of ruptured liver abscess and peritonitis.
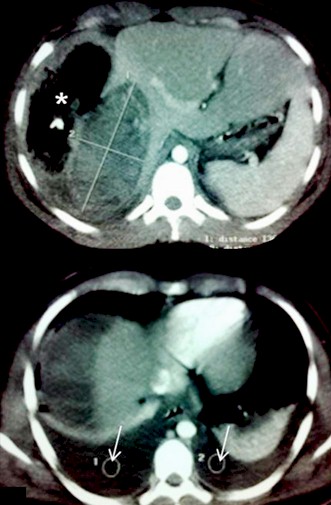
Hemoperitoneum was found with active bleeding from the liver surface. Liver wound suture was made along with perihepatic packing. The patient received five blood transfusions and was referred to our terciary care institute. On arrival the patient was unconscious and with mechanical ventilation support. Blood pressure was 70/30 mmHg, and pulse of 156 beats per minute. He had active bleeding through the surgical wound and penrose drainage. Laboratory revealed hemoglobin of 5.1 and hematocrit 15.8%. The patient underwent urgent laparotomy finding four liter hemoperitoneum and a bloody wound in right diaphragmatic hepatic surface with an approximate length of 12 cm. Liver packaging was made achieving bleeding control deciding abdominal closure. After aggressive resuscitation with intravenous fluids and massive blood transfusion he required fresh frozen plasma and packed platelets due to consumptive coagulopathy. Hemodynamic stability and corrected coagulopathy was achieved 48 hours after laparotomy. The patient underwent contrast enhanced computerized tomography showing a low density heterogeneous mass in the vast majority of the right hepatic lobe without significant peripheral enhancement due to previous surgical bleeding control. The size of the lesion was 13.6 cm for antero-posterior dimension and 6.5 for transversal measurement. Selective artery embolization of the right hepatic artery was made with ultrafluid lipiodol and gelfoam achieving flow occlusion in distal branches.
Removal of surgical packs was made twenty four hours after embolization without active bleeding documented in surgery. Enucleation was not performed due to the size of the lesion which compromised the vast majority of the right hepatic lobe requiring a posterior former hepatic resection or liver transplantation. Open drainage had minimum effusion on first recovery day and enteral nutrition was initiated via nasogastric tube. On the second day patient regained consciousness and mechanical ventilation support was not needed. Oral intake was initiated with good tolerance and progression. The patient was fully recovered and discharged on fifth day after surgery. Follow up is being made in order for definitive treatment (right hepatectomy) of the lesion without complications until date.
Images

Picture 1. Perihepatic packing for bleed control. Wound suture on right diaphragmatic liver surface. (Arrow)