Aortic stenosis and Angiodysplasia of the colon. Anesthetic- surgery priority. Case report
Aortic stenosis and Angiodysplasia of the colon. Anesthetic- surgery priority. Case report
María J. Sánchez Martin (1), Sergio Caballero Gálvez (2), Carlos García Camacho (3).
F.E.A. Anesthesia. Hospital Infantil Virgen del Rocio. Sevilla.
D.U.E. Cardiovascular Surgery- Operating Room- Clinica de Fatima. Sevilla.
D.U.E. Perfusionist. Hospital Universitario Puerta del Mar. Cadiz; Clinica de Fatima – Hospital Universitario. Sevilla.
Translation: Transworld, Language Solutions
http://www.portalesmedicos.com/traductores-medicina/transworld
Summary:
A 59-year old woman was admitted to Virgen Macarena de Sevilla Hospital by the Casualty Unit after presenting digestive hemorrhage with melenas (melanhorragia), accompanied by syncopal episodes and precordial pain. After performing complementary clinical examinations, two diagnoses are reached: Severe Aortic Stenosis and Angiodysplasia of the colon. The treatment for these two pathologies was the surgery, which gave origin to a discussion about both processes' interrelationship and the order in which they should be performed.
Introduction:
Angiodysplasia of the colon is the second cause of intestinal hemorrhage’s origin in terms of frequency order and the first cause of hemorrhage’s non determined origin after exploration and initial diagnostic tests. It consists of mucosal and submucosal vascular ectasias of the intestinal wall, which can be located all along the digestive tract. Its most frequent localizations are: cecum, ascending colon and terminal ileum.
Treatment consists of surgical resection of the bleeding area (running the risk of having new hemorrhages), endoscopic electrocoagulation, embolization and laser photocoagulation. Its association with certain grade of aortic valve stenosis is quite frequent and was initially described by Heyde1, although a clear relationship between both pathologies has not been proved yet.
Material and Method:
A 59-year old woman with antecedents of digestive hemorrhage secondary to gastric ulcus episodes goes to Hospital Virgen Macarena de Sevilla’s Casualty Unit, presenting digestive hemorrhage with melenas (melanhorragia), accompanied by syncopal episodes and precordial pain, thus we proceed to admit the patient in the hospital in order to perform clinic examinations in order to diagnose the medical profile.
Analytical assessment showed a 9.4 g/dl hemoglobin level and an 84.4 Mean Cell volume as the only alterations. The electrocardiographic study showed a left axis with disorders in the lateral face’ repolarization. A Baritado Study of the small intestine and a superior and inferior mesenteric arteriography were performed, without having found significant alterations. Grammagraphy with haematies marked for the digestive hemorrhage study was highly positive on the following 24 hours, with a possible origin in ileocecal area or angiodysplasia, affecting the splenic flexure area of the colon.
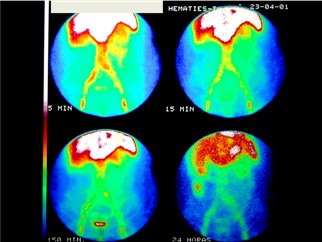
Figure 1: Grammagraphy with haematies marked for the digestive hemorrhage study.
The Echocardiogram shows a Left Ventricle hypertrophia with 18mm Septum, 12mm Posterior wall, normal Mitral valve, Aortic root at limits exceeding normality, calcified Aortic valve with severe stenosis – maximum gradient: 115 mmHg and medium gradient: 69 mmHg- and conserved ventricle function with an Ejection Fraction of 86%. After cardiac Cateterism was performed, a severe calcified aortic stenosis with normal coronary arteries was diagnosed.
Medical opinion of this medical profile was: Severe Aortic Stenosis and Angiodysplasia of the colon.
Discussion:
In clinical session, the above described case has generated a controversy since the potential risks of the two possible options were presented:
Perform a mayor abdominal surgery in a patient with critical aortic valve pathology.
Perform an aortic valve replacement with an extracorporeal circulation in a patient with a high risk of digestive haemorrhage.
In 1986, Cappel2 and Sheffer 3 described a case where intestinal bleeding ceased after aortic-valve replacement. This case poses a hypothesis on angiodysplasia etiology, as it would originate from mesenteric cellular hypoxia associated with a low cardiac output, secondary to aortic stenosis. After aortic valve replacement, the cause would be eliminated and the mesenteric vascular deficit solved.
In 1988, Imperiale et al4, performed a revision and concluded that there is not sufficient evidence that proves the cause - effect relation between the two pathologies. The cardiovascular department of the Hospital Virgen Macarena in Sevilla considers that: regardless of the degree of the stenosis, the digestive surgery has priority over valve replacement if the patient does not have severe heart failure as in the present case of study. However, if the valve pathology presupposes an immanent danger for the patient, valve replacement is then first performed.
In this case, the cardiovascular unit decided to solve the intestinal pathology by performing a terminal ileum resection and partial colectomy with mechanic ileum-colic anaestomosis in the medium third of the descending colon. Therefore, a Total Intravenous Anaesthesia (TIVA) of 120 minutes with alfentanil, rocuronium and propofol was performed where homodynamic stability remained constant at all time. After ileum- colic surgery, the digestive haemorrhage continued so an abdominal scan was repeated, where no bleeding was evident.
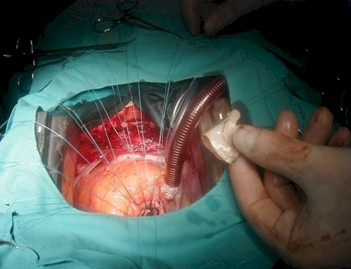
Over a period of 6 weeks, the cardiovascular unit performed an aortic valve replacement with a frame-less pericarbon bioprosthesis nº23 (fig 2 – aortic valve bio prosthesis implantation). This prosthesis was chosen to avoid post implantation anticoagulation. The anaesthetic technique used was analgesic by using remifentamil and completed with sevoflurane and cisatracurium.
The post surgery phase was good and did not present relevant complications. We believe that there should not be a standardized protocol for these cases. Which treatment has priority over the other treatment should be individual to each person, where all the healthcare services involved come to an agreement.
References:
1. HEYDE EC. Gastrointestinal bleeding in aortic stenosis. NEJM 1958; 259: 456
2. CAPPELL MS, LEBWOHL O. Cessation of recurrent bleeding from gastrointestinal angiodysplasias after aortic valve replacement. Ann Intern Med 1986 Jul;105(1):54-7
3. SCHEFFER SM, LEATHERMAN LL. Resolution of Heyde's syndrome of aortic stenosis and gastrointestinal bleeding after aortic valve replacement. Ann Thorac Surg 1986 Oct;42(4):477-80
4. IMPERIALE TF, RANSOHOFF DF. Aortic stenosis, idiopathic gastrointestinal bleeding, and angiodysplasia: is there an association? A methodologic critique of the literature. Gastroenterology 1988 Dec; 95(6):1670-6
Translation: Transworld, Language Solutions
http://www.portalesmedicos.com/traductores-medicina/transworld